Dual Stimulation IVF: How It Works, Who It’s For, and Why It’s Gaining Popularity

For individuals and couples facing challenges with conventional IVF protocols, dual stimulation IVF offers a promising alternative. This advanced fertility treatment maximizes the number of oocytes retrieved in a single menstrual cycle, making it particularly beneficial for women with low ovarian reserve or poor response to traditional ovarian stimulation. But what exactly is dual stimulation IVF, and why is it becoming an increasingly popular choice for fertility specialists and patients alike? Let’s explore the science behind this protocol, its benefits, and who may benefit most from it.
What Is Dual Stimulation IVF and Why Is It Different?
How Traditional IVF Stimulation Works
Conventional IVF relies on a single ovarian stimulation phase per menstrual cycle, typically during the follicular phase. This process involves administering hormonal medications to encourage the growth of multiple follicles, leading to the retrieval of mature eggs for fertilization. However, for women with poor ovarian response or low antral follicle count, this conventional stimulation may yield very few eggs, reducing their chances of success.
The Science Behind Dual Stimulation
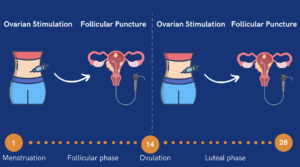
Unlike traditional IVF, dual stimulation IVF capitalizes on the fact that multiple waves of follicle recruitment occur within the same menstrual cycle. This means that even after an initial egg retrieval, the ovaries can still produce additional follicles that can be stimulated for a second retrieval.
More specifically, dual stimulation includes two distinct phases of ovarian stimulation within the same ovarian cycle: one during the follicular phase and another during the luteal phase. This double ovarian stimulation ensures that a greater number of mature oocytes are retrieved in a shorter timeframe. Research confirms that ovarian follicles continue developing across multiple waves within the same cycle, which dual stimulation IVF effectively utilizes to optimize egg retrieval.
The Shanghai Protocol: Pioneering Dual Stimulation Research
The Shanghai Protocol was a groundbreaking study that challenged traditional IVF practices by proving that ovarian stimulation could be performed twice in the same cycle. Researchers discovered that follicles continue to develop after the first egg retrieval, making a second round of stimulation and retrieval possible. This finding revolutionized treatment for poor ovarian responders, offering them a way to maximize egg retrieval within a single cycle rather than waiting for multiple cycles.
The protocol demonstrated that:
- Dual stimulation significantly increases the number of mature oocytes retrieved.
- Embryo quality from the luteal phase stimulation is comparable to that from the follicular phase.
- It is particularly beneficial for poor prognosis patients who struggle with low egg counts in conventional IVF.
As a result, the Shanghai Protocol became the foundation for modern dual stimulation approaches, leading to its adoption in fertility clinics worldwide.
Benefits of Dual Stimulation IVF and Why Does It Work
- Higher Oocyte Yield: By utilizing both follicular and luteal phase stimulations, patients can retrieve more eggs in a single cycle.
- Time Efficiency: Traditional IVF requires multiple cycles to accumulate enough eggs, whereas dual stimulation shortens the overall treatment timeline.
- Better Outcomes for Poor Responders: Research shows that poor prognosis patients benefit significantly from this approach, as it maximizes their chances of obtaining viable embryos.
Who Is Dual Stimulation IVF Best For?
Patients with Poor Ovarian Reserve or Low Egg Count
Women with diminished ovarian reserve (DOR) or a history of poor response to ovarian stimulation often struggle with retrieving an adequate number of eggs through conventional IVF. Dual stimulation is particularly beneficial for these individuals, as it leverages multiple waves of follicular growth to optimize oocyte retrieval.
Studies inspired by the Shanghai Protocol have shown that poor ovarian responders see higher cumulative embryo yields when using dual stimulation. This approach is particularly valuable for patients who have failed previous IVF cycles due to a low egg count.
Women Who Have Had Failed IVF Cycles
Patients who have previously undergone IVF with disappointing results (retrieved too few eggs for fertilization) may find dual stimulation IVF to be a more effective option. This protocol usually improves both embryo quality and quantity, which can significantly improve the chances of a successful pregnancy.
Fertility Preservation Before Medical Treatments
For individuals facing time-sensitive medical treatments, such as chemotherapy or radiation, fertility preservation is critical. Dual stimulation allows these patients to retrieve and freeze more eggs in a shorter timeframe, offering better chances for future pregnancy.
The Dual Stimulation IVF Process: Step-by-Step Guide
First Step: Follicular Phase Stimulation
The first stimulation phase begins at the start of the menstrual cycle. Patients receive gonadotropin-releasing hormone agonists and luteinizing hormone to stimulate the growth of multiple follicles in the ovaries. These medications encourage the follicles to mature simultaneously, increasing the chances of retrieving a greater number of viable eggs.
Once the follicles reach an optimal size, a trigger shot of human chorionic gonadotropin (hCG) or a GnRH agonist is administered to finalize egg maturation. Around 36 hours later, the first oocyte retrieval takes place, where a specialist extracts the mature eggs using a minimally invasive ultrasound-guided procedure.
Second Step: Luteal Phase Stimulation
Immediately after the first egg retrieval, the second phase of stimulation begins. Unlike conventional protocols that wait for a new cycle, dual stimulation utilizes the second wave of follicular growth that occurs within the same menstrual cycle.
During this luteal phase stimulation, adjusted doses of gonadotropins and other fertility medications are used to encourage a new set of follicles to mature. These follicles, although developed later, have been shown to produce eggs of comparable quality to those retrieved during the follicular phase.
Once the second set of follicles reaches maturity, another oocyte retrieval is performed. This allows the patient to collect two batches of eggs within a single cycle, maximizing the chances of success.
What Happens Next?
After both retrievals, the collected embryos can be frozen or transferred depending on the patient’s treatment plan. Many fertility specialists recommend freezing the embryos for later use, as it allows for genetic testing (PGT-A) and better preparation for implantation.
Risks, Challenges, and What to Expect During Dual Stimulation IVF
Physical Side Effects and How to Manage Them
Because dual stimulation IVF involves two rounds of ovarian stimulation in the same cycle, the body undergoes an increased hormonal load compared to conventional IVF. This can lead to various physical side effects, some of which may be more intense due to the double stimulation.
Common Physical Symptoms
- Bloating and Abdominal Discomfort: The ovaries become enlarged due to the hormone-induced follicle growth, which can cause feelings of heaviness, cramping, and bloating.
- Fatigue: Hormonal changes can make patients feel more tired than usual, especially during the second stimulation phase.
- Ovarian Discomfort or Pain: Some women experience sharp or dull pain in the pelvic area, particularly after egg retrievals.
- Hormonal Shifts: Emotional fluctuations, mood swings, headaches, and nausea can result from changing hormone levels during stimulation.
How to Manage These Side Effects
- Stay Hydrated: Drinking plenty of fluids, especially electrolyte-rich drinks, can help reduce bloating and fatigue.
- Rest and Listen to Your Body: Overexertion can worsen symptoms, so it’s best to take it easy and allow time for recovery after retrievals.
- Dietary Adjustments: Eating light, protein-rich foods can help manage nausea and bloating.
- Pain Management: Over-the-counter pain relievers like acetaminophen can help ease discomfort, but always consult your fertility specialist before taking any medications.
- Monitor for OHSS (Ovarian Hyperstimulation Syndrome): While dual stimulation is highly effective, some studies suggest it requires careful monitoring to minimize the risk of ovarian hyperstimulation syndrome (OHSS). If severe bloating, rapid weight gain, and difficulty breathing arise, immediate medical attention is necessary.
Financial and Emotional Considerations
Undergoing dual stimulation IVF is a significant financial and emotional commitment. Compared to traditional IVF, it involves additional medications, monitoring appointments, and egg retrievals, making it more expensive. Moreover, the emotional toll of back-to-back stimulation cycles can be overwhelming for some patients.
Cost Considerations
- Higher Medication Costs: Because two rounds of stimulation are involved, patients need more hormone injections, which can increase costs significantly.
- More Frequent Monitoring Appointments: Additional ultrasounds and blood tests are required to track follicular development in both phases.
- Insurance Coverage: Many insurance plans only cover a portion of IVF treatments, so it’s important to check whether dual stimulation is included.
- Long-Term Savings: While dual stimulation IVF may be more expensive upfront, it can actually be more cost-effective in the long run by reducing the number of cycles needed to retrieve enough eggs.
Emotional and Mental Health Challenges
- Increased Emotional Strain: Hormonal fluctuations combined with the stress of treatment can lead to heightened anxiety, irritability, or mood swings.
- The Pressure to Succeed: Many patients undergoing dual stimulation IVF are those who have already had failed cycles, which can intensify feelings of desperation or fear of another failure.
- Coping with Physical Exhaustion: Two back-to-back stimulations in a short timeframe can be physically draining.
How to Cope with the Emotional Toll
- Seek Support: Talking to a fertility counselor, therapist, or joining an online support group can help process emotions.
- Mindfulness and Stress Reduction: Practices like meditation, yoga, and acupuncture may provide relief and improve overall well-being during the process.
- Partner and Family Involvement: Having a strong support system in place can help reduce the burden and make the journey more manageable.
- Focus on the End Goal: While the journey may be challenging, keeping sight of the long-term goal (a successful pregnancy) can help patients stay motivated.
Addressing Concerns About Egg Quality
Some patients worry that eggs retrieved during the luteal phase might be of lower quality compared to those from the follicular phase. However, extensive research, including findings from the Shanghai Protocol, suggests that embryos obtained from both phases have comparable developmental potential. This means that luteal phase stimulation does not compromise success rates and is a viable approach for maximizing egg retrieval.
Comparing Dual Stimulation IVF vs. Conventional IVF: Which Is More Effective?
Number of Eggs Retrieved: Why It Matters
One of the primary challenges for patients with low ovarian reserve or poor ovarian response is the limited number of eggs retrieved during each IVF cycle. Since egg quantity is a crucial factor in IVF success, the ability to retrieve more eggs in a single cycle can greatly improve a patient’s chances of fertilization and embryo development.
- Conventional IVF: Typically yields a limited number of mature oocytes per cycle, particularly for poor responders who may only retrieve a few eggs.
- Dual Stimulation IVF: Allows for two retrievals within the same menstrual cycle, significantly increasing the total number of mature oocytes collected.
- Why It Matters: More retrieved eggs increase the likelihood of obtaining viable embryos, which can be used for fresh or frozen transfers or preimplantation genetic testing (PGT-A) to identify chromosomally normal embryos.
For patients with low ovarian reserve, maximizing each cycle’s output is crucial. Dual stimulation provides a more aggressive approach to ensure no opportunity for egg retrieval is missed. Recent studies show that dual stimulation IVF leads to a higher cumulative embryo yield than conventional protocols, making it a compelling option for poor responders (Fertility and Sterility, 2024).
Time Efficiency: Fewer Cycles, Faster Results
The standard IVF process can be lengthy, often requiring multiple cycles to accumulate enough eggs for a successful pregnancy. This prolonged timeline can be frustrating, costly, and emotionally draining for patients who already have difficulty responding to stimulation.
- Conventional IVF: Requires waiting for a new menstrual cycle after each retrieval, leading to months or even years of treatment.
- Dual Stimulation IVF: Eliminates the waiting period between cycles by retrieving eggs twice in one cycle, reducing the overall treatment timeline.
- Why It Matters: Patients who need to move quickly (such as those pursuing fertility preservation before cancer treatments) benefit greatly from retrieving more eggs in a shorter period.
By reducing the number of cycles needed, dual stimulation IVF also lowers the overall emotional and physical toll on patients, allowing them to progress toward embryo transfer sooner.
Success Rates: Does Dual Stimulation Lead to More Pregnancies?
Ultimately, the goal of any IVF treatment is a successful pregnancy, and research suggests that dual stimulation IVF can offer a distinct advantage in this regard, particularly for poor ovarian responders.
- Higher Cumulative Embryo Numbers: Since dual stimulation increases the number of eggs retrieved, it naturally leads to more embryos available for transfer.
- Better Embryo Selection: A higher embryo count allows for better selection, increasing the chances of transferring a chromosomally normal embryo with a high implantation potential.
- Why Poor Responders Benefit More: Studies show that patients with a history of low egg retrieval in conventional IVF see higher live birth rates when using dual stimulation.
Additionally, by reducing the need for repeated ovarian stimulation cycles, dual stimulation IVF allows patients to undergo fewer total treatments while achieving the same or better pregnancy success rates.
Is Dual Stimulation IVF Right for You?
If you’ve been struggling with low ovarian reserve, poor response to traditional IVF, or previous failed cycles, dual stimulation IVF could offer you a new path forward. This innovative protocol is designed to maximize your chances of retrieving viable eggs, helping you create more embryos in a shorter period of time.
But fertility isn’t one-size-fits-all, and the best way to know if dual stimulation IVF is right for you is to speak with a fertility specialist who understands your unique journey. Our expert team is here to provide personalized guidance, answer your questions, and create a treatment plan tailored to your needs.
You don’t have to navigate this journey alone. Schedule a consultation with our clinic today, and let’s explore the best fertility options for you. Your dream of starting or growing your family is still within reach. We’re here to help you get there!